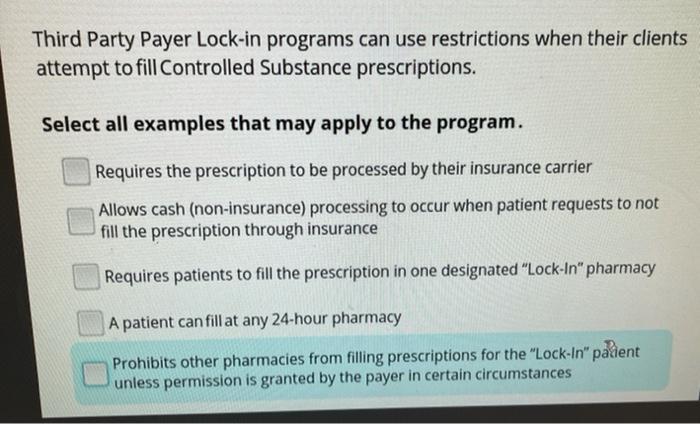
Third party payer lock-in programs can use restrictions – Third-party payer lock-in programs can use restrictions to limit patient access to preferred providers and treatment options, creating barriers to entry for new providers and stifling innovation in healthcare delivery. This raises concerns about patient autonomy, the doctor-patient relationship, market competition, and the overall cost and quality of healthcare services.
Understanding the implications of these programs is crucial for policymakers, healthcare providers, and patients alike. This comprehensive analysis delves into the impact of third-party payer lock-in programs on patient choice, market competition, cost implications, ethical considerations, and regulatory and policy implications.
Impact on Patient Choice
Third-party payer lock-in programs can significantly limit patient access to preferred providers and treatment options. These programs typically establish a network of providers that patients must use to receive covered services. As a result, patients may be unable to see their preferred doctors or receive care from providers who specialize in their specific condition.
For example, a patient with a rare disease may be unable to find a specialist within their insurer’s network. This can delay diagnosis and treatment, potentially leading to worse health outcomes. Additionally, patients may be forced to travel long distances or pay out-of-pocket costs to access care from providers outside of the network.
These restrictions can also impact patient autonomy and the doctor-patient relationship. Patients may feel pressured to choose providers based on their insurance coverage rather than their medical needs. This can erode trust between patients and their doctors and make it more difficult for patients to make informed decisions about their healthcare.
Market Competition and Innovation

Third-party payer lock-in programs can stifle competition within the healthcare industry. By creating barriers to entry for new providers, these programs make it more difficult for smaller or independent providers to compete with larger, established providers.
This lack of competition can lead to higher prices, lower quality of care, and reduced innovation. Providers may have less incentive to improve their services or develop new treatments if they know that patients are locked into their network.
Additionally, third-party payer lock-in programs can discourage innovation by limiting the ability of new providers to enter the market. Startups and small businesses may be unable to compete with the large, established providers that are already part of the network.
Cost Implications
Third-party payer lock-in programs can have significant cost implications for patients, providers, and the healthcare system as a whole.
For patients, these programs can lead to higher out-of-pocket costs. Patients may be forced to pay for services that are not covered by their insurance or to travel long distances to access care from providers outside of the network.
For providers, third-party payer lock-in programs can lead to lower reimbursement rates and increased administrative costs. Providers may have to spend more time negotiating with insurers and dealing with paperwork, which can take away from patient care.
For the healthcare system as a whole, third-party payer lock-in programs can lead to increased healthcare spending. These programs can create inefficiencies and increase the cost of care for everyone.
Ethical Considerations
Third-party payer lock-in programs raise a number of ethical concerns. These programs can create conflicts of interest between insurers and patients, as insurers may have an incentive to limit access to care in order to reduce costs.
Additionally, these programs can impact patient well-being by limiting access to necessary care. Patients may be forced to delay or forego treatment due to the restrictions imposed by their insurance coverage.
Finally, third-party payer lock-in programs can erode the fiduciary responsibilities of healthcare providers. Providers may be pressured to make decisions based on the financial interests of the insurer rather than the best interests of the patient.
Regulatory and Policy Implications
The existing regulatory landscape governing third-party payer lock-in programs is complex and varies from state to state. Some states have laws that prohibit insurers from restricting patient access to care, while other states have no such laws.
There is a growing movement to address the concerns associated with third-party payer lock-in programs. Several states have passed laws that require insurers to provide patients with more information about their network of providers and to allow patients to appeal denials of coverage.
The federal government is also considering action to address this issue. The Centers for Medicare & Medicaid Services (CMS) has proposed a rule that would prohibit insurers from using lock-in programs to restrict patient access to care.
Helpful Answers: Third Party Payer Lock-in Programs Can Use Restrictions
What are the primary concerns with third-party payer lock-in programs?
Third-party payer lock-in programs raise concerns about limiting patient choice, stifling competition, increasing costs, and compromising ethical considerations in healthcare.
How do these programs impact patient choice?
They can restrict patients’ access to preferred providers and treatment options, potentially affecting their autonomy and the doctor-patient relationship.
What are the implications for healthcare innovation?
Lock-in programs can create barriers to entry for new providers and stifle innovation in healthcare delivery, potentially reducing the quality and accessibility of services.